It's not your imagination: Picking the right birth control is more confusing at this age than ever. "There are more options for over-35 women now," says Dr. Andrew M. Kaunitz, professor and associate chairman of OB/GYN at the University of Florida College of Medicine—Jacksonville.
 Don't look at that as overwhelming—it means there's a method out there that's not only safe, but right for your life. We investigated them all to help you choose the very best way for you to go.
Don't look at that as overwhelming—it means there's a method out there that's not only safe, but right for your life. We investigated them all to help you choose the very best way for you to go.
If you're done having kids—at least for now:
What to pick when you're pretty sure you're done with babymaking? Here's what doctors recommend in order of preference:
Intrauterine device (IUD) or implant. Our experts love long-acting reversible contraception—namely an IUD or implant. Last year, the American Congress of Obstetricians and Gynecologists recommended them over every other reversible contraception available. That's because they're nearly as effective as permanent birth control (i.e., getting your tubes tied), but you can remove them if you want to get pregnant, explains Dr. Deborah Nucatola, senior director of medical services for Planned Parenthood Federation of America. Bonus if you're over 40:
"As you approach menopause, you're more likely to have heavy periods, and the IUD can be useful in controlling the bleeding," Kaunitz explains.
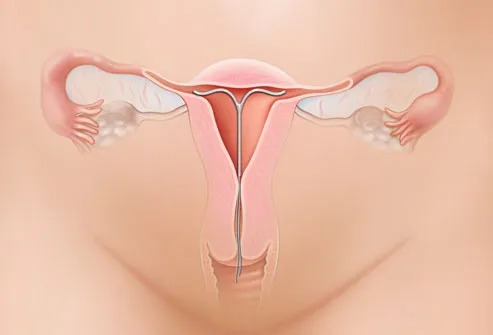 There are two types of IUDs:
There are two types of IUDs:
* The Mirena releases progestin and can be worn up to five years; after some initial spotting, it makes your period much lighter.
* ParaGard (which is made of copper, so steer clear if you're allergic) is hormone-free and can actually make your periods heavier for the first few months. The upside? It lasts up to 10 years. Some women may experience temporary pain, bleeding, or ovarian cysts after getting either type of IUD. Very rarely, an IUD could tear the uterine lining.
The two types of implants are Nexplanon and Implanon, which go into your arm (you'll see a small bump under your skin). They're good for three years. Like the hormonal IUD, they release progestin. While these long-acting options are pricey at the outset, paying for the Pill over decades can cost just as much, or more. Cost: $500 to $1,000 for IUDs and $400 to $800 for implants.
___________________________________________________
More From Health.com:
12 Types of Birth Control
7 Common Birth Control Side Effects
16 Worst Birth Control Mistakes
__________________________________________________
 The Pill. Want to stay on it (or start)? No worries: As long as you're at a healthy weight, don't smoke, and don't suffer from high blood pressure, diabetes, or migraines, you can safely take the combination estrogen/progestin Pill until age 55, Kaunitz says. Same goes for the Patch and the Ring. Though all three methods slightly raise your risk of blood clots, that risk is still lower than your odds of clotting should you get pregnant, he points out.
The Pill. Want to stay on it (or start)? No worries: As long as you're at a healthy weight, don't smoke, and don't suffer from high blood pressure, diabetes, or migraines, you can safely take the combination estrogen/progestin Pill until age 55, Kaunitz says. Same goes for the Patch and the Ring. Though all three methods slightly raise your risk of blood clots, that risk is still lower than your odds of clotting should you get pregnant, he points out.
Perks of the Pill: It can ease PMS symptoms and adult acne, reduce hot flashes, lower your risk for endometrial and ovarian cancer, and provide protection from osteoporosis. (And no, it doesn't raise your breast cancer risk.) If you have health issues that make the combination pill risky, consider the progestin-only mini pill instead. Cost: $15 to $80 a month.
If you're single with an active sex life:
Condoms. Unless you're in a mutually monogamous relationship, using these is the only way to protect against sexually transmitted diseases. Because a decline in estrogen as you age can dry you out, you may need extra lubrication—water-based, since oil-based lubes can damage condoms, Nucatola notes. (Don't rely on the rhythm method; irregular periods leading up to menopause make it unreliable.) Cost: About $1 each.
If you're sure you don't want more kids:
Sterilization. Though it might sound like a last resort, sterilization is actually the most popular form of birth control among women over 35, a new study shows. And for good reason: It's safe, effective, and permanent—no worries about "oops" pregnancies, or even thinking about contraception ever again. The traditional choice is tubal ligation surgery, in which a doctor makes a small incision in your abdomen while you're under anesthesia, then ties off or blocks your fallopian tubes. You'll need a week to recover.
 Then there are Adiana and Essure—tiny inserts made of silicone or metal, respectively, that are placed into your tubes, blocking fertilization. You won't need anesthesia or an incision, and recovery takes less than a week. Unlike the tubal—which works instantly—inserts take at least three months to block fertilization, so use a backup method until then. These methods are also far more difficult to reverse than the surgery. Cost: $1,500 to $6,000.
Then there are Adiana and Essure—tiny inserts made of silicone or metal, respectively, that are placed into your tubes, blocking fertilization. You won't need anesthesia or an incision, and recovery takes less than a week. Unlike the tubal—which works instantly—inserts take at least three months to block fertilization, so use a backup method until then. These methods are also far more difficult to reverse than the surgery. Cost: $1,500 to $6,000.
Concerned about the cost factor of contraception? There's less reason to be these days. Under the 2012 Affordable Care Act, most birth control is now covered by insurance. (You may still have a co-pay, though, so check with your insurer.) Bottom line: More options plus better reimbursement equal less stress about getting the protection you need.
Should he get snipped?
Maybe it's time for him to take a birth-control bullet for the team by getting a vasectomy, in which a doctor makes a small incision or puncture in the scrotum, then cuts or ties the vas deferens tubes so sperm can't travel into the semen. Recovery takes just a few days and isn't very painful (though, considering that only about 5 percent of married men have gotten one, your guy may not believe that!). Vasectomies can typically be reversed, but not always. You'll need backup birth control for three months post-procedure, until a test confirms that he's shooting blanks. Cost: $350 to $1,000.
Birth control right after baby:
Most women get the green light to have sex again after their six-week postpartum checkup. What to know when you're ready to get back in the saddle:
Breast-feeding exclusively does block ovulation, but it's not foolproof, so consider using a backup method (and lots of lube, since the hormones released by nursing will make you very dry).
 Diaphragms you used pre-baby should be tossed post-delivery. "Your old one may not fit anymore," Nucatola says. Get fitted for a new one.
Diaphragms you used pre-baby should be tossed post-delivery. "Your old one may not fit anymore," Nucatola says. Get fitted for a new one.
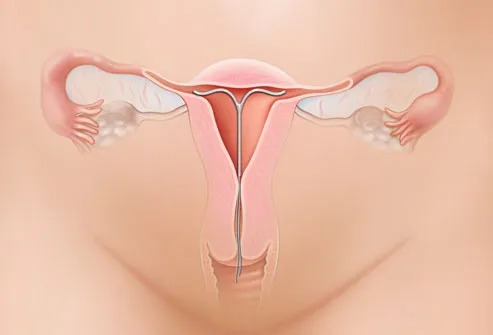
Mini pills are a better choice right now than the combination pill, which can hamper milk production. IUDs (shown) can't go in until your uterus shrinks back to its normal size—which happens, conveniently, around your six-week check. If you're interested, call your doc in advance and ask him to insert one during your visit.
 Don't look at that as overwhelming—it means there's a method out there that's not only safe, but right for your life. We investigated them all to help you choose the very best way for you to go.
Don't look at that as overwhelming—it means there's a method out there that's not only safe, but right for your life. We investigated them all to help you choose the very best way for you to go.If you're done having kids—at least for now:
What to pick when you're pretty sure you're done with babymaking? Here's what doctors recommend in order of preference:
Intrauterine device (IUD) or implant. Our experts love long-acting reversible contraception—namely an IUD or implant. Last year, the American Congress of Obstetricians and Gynecologists recommended them over every other reversible contraception available. That's because they're nearly as effective as permanent birth control (i.e., getting your tubes tied), but you can remove them if you want to get pregnant, explains Dr. Deborah Nucatola, senior director of medical services for Planned Parenthood Federation of America. Bonus if you're over 40:
"As you approach menopause, you're more likely to have heavy periods, and the IUD can be useful in controlling the bleeding," Kaunitz explains.
 There are two types of IUDs:
There are two types of IUDs:* The Mirena releases progestin and can be worn up to five years; after some initial spotting, it makes your period much lighter.
* ParaGard (which is made of copper, so steer clear if you're allergic) is hormone-free and can actually make your periods heavier for the first few months. The upside? It lasts up to 10 years. Some women may experience temporary pain, bleeding, or ovarian cysts after getting either type of IUD. Very rarely, an IUD could tear the uterine lining.
The two types of implants are Nexplanon and Implanon, which go into your arm (you'll see a small bump under your skin). They're good for three years. Like the hormonal IUD, they release progestin. While these long-acting options are pricey at the outset, paying for the Pill over decades can cost just as much, or more. Cost: $500 to $1,000 for IUDs and $400 to $800 for implants.
___________________________________________________
More From Health.com:
12 Types of Birth Control

7 Common Birth Control Side Effects

16 Worst Birth Control Mistakes

__________________________________________________
 The Pill. Want to stay on it (or start)? No worries: As long as you're at a healthy weight, don't smoke, and don't suffer from high blood pressure, diabetes, or migraines, you can safely take the combination estrogen/progestin Pill until age 55, Kaunitz says. Same goes for the Patch and the Ring. Though all three methods slightly raise your risk of blood clots, that risk is still lower than your odds of clotting should you get pregnant, he points out.
The Pill. Want to stay on it (or start)? No worries: As long as you're at a healthy weight, don't smoke, and don't suffer from high blood pressure, diabetes, or migraines, you can safely take the combination estrogen/progestin Pill until age 55, Kaunitz says. Same goes for the Patch and the Ring. Though all three methods slightly raise your risk of blood clots, that risk is still lower than your odds of clotting should you get pregnant, he points out.Perks of the Pill: It can ease PMS symptoms and adult acne, reduce hot flashes, lower your risk for endometrial and ovarian cancer, and provide protection from osteoporosis. (And no, it doesn't raise your breast cancer risk.) If you have health issues that make the combination pill risky, consider the progestin-only mini pill instead. Cost: $15 to $80 a month.
If you're single with an active sex life:
Condoms. Unless you're in a mutually monogamous relationship, using these is the only way to protect against sexually transmitted diseases. Because a decline in estrogen as you age can dry you out, you may need extra lubrication—water-based, since oil-based lubes can damage condoms, Nucatola notes. (Don't rely on the rhythm method; irregular periods leading up to menopause make it unreliable.) Cost: About $1 each.
If you're sure you don't want more kids:
Sterilization. Though it might sound like a last resort, sterilization is actually the most popular form of birth control among women over 35, a new study shows. And for good reason: It's safe, effective, and permanent—no worries about "oops" pregnancies, or even thinking about contraception ever again. The traditional choice is tubal ligation surgery, in which a doctor makes a small incision in your abdomen while you're under anesthesia, then ties off or blocks your fallopian tubes. You'll need a week to recover.
 Then there are Adiana and Essure—tiny inserts made of silicone or metal, respectively, that are placed into your tubes, blocking fertilization. You won't need anesthesia or an incision, and recovery takes less than a week. Unlike the tubal—which works instantly—inserts take at least three months to block fertilization, so use a backup method until then. These methods are also far more difficult to reverse than the surgery. Cost: $1,500 to $6,000.
Then there are Adiana and Essure—tiny inserts made of silicone or metal, respectively, that are placed into your tubes, blocking fertilization. You won't need anesthesia or an incision, and recovery takes less than a week. Unlike the tubal—which works instantly—inserts take at least three months to block fertilization, so use a backup method until then. These methods are also far more difficult to reverse than the surgery. Cost: $1,500 to $6,000.Concerned about the cost factor of contraception? There's less reason to be these days. Under the 2012 Affordable Care Act, most birth control is now covered by insurance. (You may still have a co-pay, though, so check with your insurer.) Bottom line: More options plus better reimbursement equal less stress about getting the protection you need.
Should he get snipped?
Maybe it's time for him to take a birth-control bullet for the team by getting a vasectomy, in which a doctor makes a small incision or puncture in the scrotum, then cuts or ties the vas deferens tubes so sperm can't travel into the semen. Recovery takes just a few days and isn't very painful (though, considering that only about 5 percent of married men have gotten one, your guy may not believe that!). Vasectomies can typically be reversed, but not always. You'll need backup birth control for three months post-procedure, until a test confirms that he's shooting blanks. Cost: $350 to $1,000.
Birth control right after baby:
Most women get the green light to have sex again after their six-week postpartum checkup. What to know when you're ready to get back in the saddle:
Breast-feeding exclusively does block ovulation, but it's not foolproof, so consider using a backup method (and lots of lube, since the hormones released by nursing will make you very dry).
 Diaphragms you used pre-baby should be tossed post-delivery. "Your old one may not fit anymore," Nucatola says. Get fitted for a new one.
Diaphragms you used pre-baby should be tossed post-delivery. "Your old one may not fit anymore," Nucatola says. Get fitted for a new one.Mini pills are a better choice right now than the combination pill, which can hamper milk production. IUDs (shown) can't go in until your uterus shrinks back to its normal size—which happens, conveniently, around your six-week check. If you're interested, call your doc in advance and ask him to insert one during your visit.

0 comments:
Post a Comment